Towards Establishing Standards of Care of Injection Therapies for Pain Management Delivered by Integrative Healthcare Providers
Naturopathic doctors practicing interventional orthopedics in provinces and states with a broad scope of practice are perfectly positioned to offer high quality interventional pain management care. Current injection training for NDs varies greatly depending on which state or province they are licensed in. NDs in North America primarily use landmark guided injections of orthobiologics (platelet rich plasma (PRP) and stem cells), prolotherapy, neural, and perineural injections. To further advance our profession in this field, a focus on diagnostic accuracy, competent delivery of image-guided procedural-based interventions, and the addition of hyaluronic acid and the judicious use of corticosteroids is warranted.
Over the last 10 years the scope of naturopathic physicians in North America has markedly broadened. This progression in scope has afforded opportunities for naturopathic doctors to practice non-surgical orthopedic interventions using a variety of orthobiologic and pharmaceutical agents. The most recent naturopathic scope expansion happened in the Northwest Territories (NWT), Canada. As of March 1st, 2022, naturopathic physicians in NWT were given full practicing scope and coverage under the Health and Social Services Professions Act allowing the ability to diagnose and treat pathology, prescription authority, and license to perform in-office minor surgery and interventional orthopedic injection procedures. Table 1 showcases jurisdictions across North America that allow NDs to perform injection therapies for pain management and various considerations specific to each state/province.
Table 1. Jurisdictions Across North America that Allow Injection Therapies for Pain Management by Naturopathic Doctors
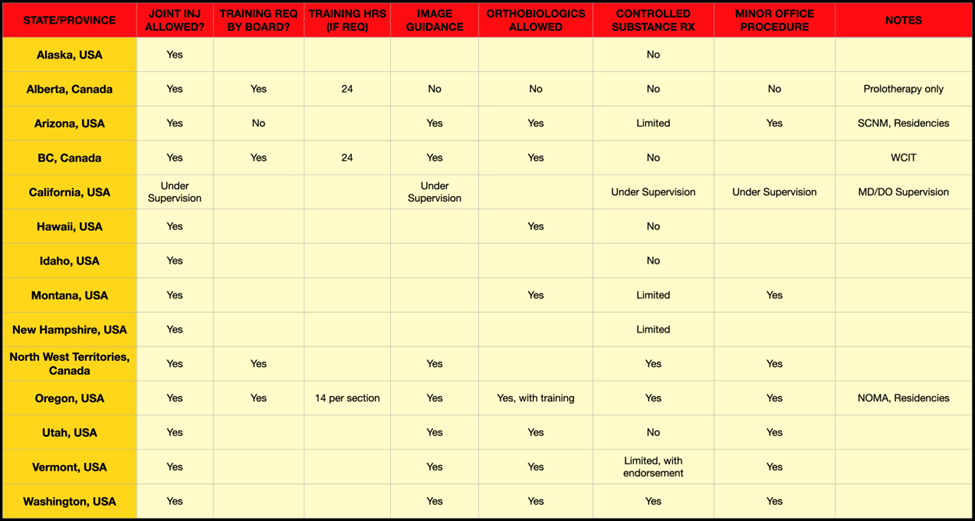
Abbreviations
Joint Inj Allowed?: Are joint injections allowed in this state or province by NDs?
Training Req By Board?: If joint injections are allowed, does the governing board require training before the ND performs joint injections?
Training Hrs (If Req): If training is required, how many hours?
Image Guidance: Are NDs allowed to use ultrasound or fluoroscopy to guide the needle when they do joint injections?
Orthobiologics Allowed: Are NDs allowed to harvest and/or use injectate made from the patient’s own blood products, such as platelet-rich plasma, micronized fat, or bone marrow aspirate concentrate? Some jurisdictions may allow one or more of these injectates and may or may not allow the harvesting of such injectate.
Controlled Substance RX: Are NDs allowed to prescribe controlled substances in any capacity? This varies based on state/province.
Minor Office Procedure: Are NDs allowed to perform in-office minor surgical procedures, as outlined by the statutes written by each jurisdiction’s board?
Notes: May include information about residencies, advocacy groups, special rules, or anything else.
As the naturopathic scope continues to broaden and the number of professional registrants grows, the need for standardization in diagnostic training, image guidance, and interventional pain protocols would benefit the profession. These standards will help to ensure that naturopathic doctors use evidence-based interventions, maintain public safety, and optimize therapeutic outcomes.
Enhancing the fundamental skill set of professionals requires agreement between all stakeholders, including institutional support from both private and public entities and interprofessional collaboration for the development and delivery of standardized protocols. In the absence of standardized application of current evidence-based protocols, it might be easy for the naturopathic profession to settle into long-held approaches for treating pain that have more to do with tradition and historical lack of pharmaceutical access than delivering comprehensive interventional orthopedic care.
As licensed and regulated healthcare providers, naturopathic doctors are able to communicate a diagnosis to patients using case history, clinical presentations, and use of laboratory and imaging modalities. To ensure therapeutic success, the importance of an accurate diagnosis should be the primacy of all healthcare providers prior to treatment. Providers unsure of their diagnosis should work with the patient to formulate a plan to get to a diagnosis through a diagnostic injection, further exam or imaging, or referral to another provider.
Point-of-care ultrasound (POCUS) can assist with both in-office assessment and procedural intervention. Ultrasound is not a replacement for traditional diagnostic imaging, however, it is useful on superficial tissues such as for subacromial bursa and rotator cuff assessment. Ultrasound is superior for needle guidance yielding improved accuracy, safety, and efficacy (Lee and Griffith 2019, Lin et al 2021, Strakowski and Visco 2019).
The use of image guidance for therapeutic injection began to receive significant research attention approximately a decade ago. The theoretical advantage of image guided injections was obvious, yet concerns were raised that the strategy would be blindly adopted without proper rigor in evaluation of relative efficacy to the standard of care- landmark guided injection (Bloom et al 2012, Rathmell et al 2012, Sage et al 2013). The past decade has witnessed hundreds of human trials comparing safety and efficacy of image guided versus landmark guided injection for pain management. Numerous meta analyses have concluded that image guided therapy is superior to landmark guided (Fang et al 2021, Gutierrez et al 2016, Hoeber et al 2016, Li et al 2014, Rimeika et al 2021, Sakellariou et al 2017, Wang et al 2021, Wu et al 2015, Yang et al 2021).
The American Medical Society for Sports Medicine published a position statement in 2015 addressing ultrasound guided injection therapy for pain management. Ultrasound guided injections were concluded to be more accurate than landmark guided injections (Evidence Rating=A), more efficacious (Evidence Rating=B), and required to perform many new procedures (Evidence Rating=C) (Finnoff et al 2015). The orthopedic use of corticosteroids is underutilized in the naturopathic profession despite there being a large body of evidence for its clinical utility and its ubiquitous use in conventional care (Ayub et al 2021, Chen et al 2019, Jiang et al 2020, Jüni et al 2015, Marsland et al 2014). The judicious use of steroids should play an important role in interventional orthopedic practice, for example, in the case of a person living with chronic pain while waiting for replacement arthroplasty (McMahon et al 2013 Pereira et al 2016). A corticosteroid injection can also be very helpful as a diagnostic injection, reducing inflammation and pain long enough to help identify the source of pain generation. Further, many patients are not interested in getting numerous injections over multiple treatments of prolotherapy or PRP for reasons of cost and comfort. While corticosteroids certainly come with risks, most notably accelerated tissue degeneration, banishing them from an interventional orthopedic practice translates to helping fewer people.
Hyaluronic acid injections, like corticosteroids, are Health Canada and FDA approved to treat joint pain secondary to osteoarthritis. Hyaluronic acid may reduce inflammation and friction to slow the degeneration of cartilage and bone, making it a prevention-based treatment for those living with osteoarthritic pain (Bannuru et al 2011, He et al 2017). This injectable therapeutic option has demonstrated pain relief in those living with grades 1-3 osteoarthritis in both the hip and knee (McGrath et al 2013). With additional coverage from insurance agencies, this therapeutic can also be a more affordable option than other therapies such as Platelet-Rich Plasma.
In developing this preamble to our joint position statement on injection therapy, we have collaborated with clinicians in the field of interventional orthopedics from a range of disciplines including allopathic medicine, chiropractic medicine, physiotherapy, and naturopathic medicine. It is our hope that all stakeholders in naturopathic medicine will join us in advancing the standardization of both physician skills and injection protocols in the naturopathic profession.
References
Ayub S, Kaur J, Hui M, Espahbodi S, Hall M, Doherty M, Zhang W. Efficacy and safety of multiple intra-articular corticosteroid injections for osteoarthritis-a systematic review and meta-analysis of randomized controlled trials and observational studies. Rheumatology (Oxford). 2021 Apr 6;60(4):1629-1639.
Bannuru RR, Natov NS, Dasi UR, Schmid CH, McAlindon TE. Therapeutic trajectory following intra-articular hyaluronic acid injection in knee osteoarthritis–meta-analysis. Osteoarthritis Cartilage. 2011 Jun;19(6):611-619.
Bloom JE, Rischin A, Johnston RV, Buchbinder R. Image-guided versus blind glucocorticoid injection for shoulder pain. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD009147.
Chen R, Jiang C, Huang G. Comparison of intra-articular and subacromial corticosteroid injection in frozen shoulder: A meta-analysis of randomized controlled trials. Int J Surg. 2019 Aug;68:92-103.
Fang WH, Chen XT, Vangsness CT Jr. Ultrasound-Guided Knee Injections Are More Accurate Than Blind Injections: A Systematic Review of Randomized Controlled Trials. Arthrosc Sports Med Rehabil. 2021 Jun 26;3(4):e1177-e1187.
Finnoff JT, Hall MM, Adams E, Berkoff D, Concoff AL, Dexter W, Smith J; American Medical Society for Sports Medicine. American Medical Society for Sports Medicine position statement: interventional musculoskeletal ultrasound in sports medicine. Clin J Sport Med. 2015 Jan;25(1):6-22.
Gutierrez M, Di Matteo A, Rosemffet M, Cazenave T, Rodriguez-Gil G, Diaz CH, Rios LV, Zamora N, Guzman Mdel C, Carrillo I, Okano T, Salaffi F, Pineda C; Pan-American League against Rheumatisms (PANLAR) Ultrasound Study Group. Short-term efficacy to conventional blind injection versus ultrasound-guided injection of local corticosteroids in tenosynovitis in patients with inflammatory chronic arthritis: A randomized comparative study. Joint Bone Spine. 2016 Mar;83(2):161-6.
He WW, Kuang MJ, Zhao J, Sun L, Lu B, Wang Y, Ma JX, Ma XL. Efficacy and safety of intraarticular hyaluronic acid and corticosteroid for knee osteoarthritis: A meta-analysis. Int J Surg. 2017 Mar;39:95-103.
Hoeber S, Aly AR, Ashworth N, Rajasekaran S. Ultrasound-guided hip joint injections are more accurate than landmark-guided injections: a systematic review and meta-analysis. Br J Sports Med. 2016 Apr;50(7):392-6.
Jiang M, Lim K, Nikpour M. Safety of Intra-articular Corticosteroid Injection. Radiology. 2020 Mar;294(3):720-722.
Jüni P, Hari R, Rutjes AW, Fischer R, Silletta MG, Reichenbach S, da Costa BR. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev. 2015 Oct 22;2015(10):CD005328
Lee RKL, Griffith JF. Top-Ten Tips for Ultrasound-Guided Joint Injection. Semin Musculoskelet Radiol. 2019 Aug;23(4):419-428.
Li Z, Xia C, Yu A, Qi B. Ultrasound- versus palpation-guided injection of corticosteroid for plantar fasciitis: a meta-analysis. PLoS One. 2014 Mar 21;9(3):e92671.
Lin JS, Gimarc DC, Adler RS, Beltran LS, Merkle AN. Ultrasound-Guided Musculoskeletal Injections. Semin Musculoskelet Radiol. 2021 Dec;25(6):769-784.
Marsland D, Mumith A, Barlow IW. Systematic review: the safety of intra-articular corticosteroid injection prior to total knee arthroplasty. Knee. 2014 Jan;21(1):6-11.
McGrath AF, McGrath AM, Jessop ZM, Gandham S, Datta G, Dawson-Bowling S, Cannon SR. A comparison of intra-articular hyaluronic acid competitors in the treatment of mild to moderate knee osteoarthritis. J Arthritis. 2013;2(1):1000108.
McMahon SE, LeRoux JA, Smith TO, Hing CB. Total joint arthroplasty following intra-articular steroid injection: a literature review. Acta Orthop Belg. 2013 Dec;79(6):672-679.
Pereira LC, Kerr J, Jolles BM. Intra-articular steroid injection for osteoarthritis of the hip prior to total hip arthroplasty: is it safe? a systematic review. Bone Joint J. 2016 Aug;98-B(8):1027-1035.
Rathmell JP, Manion SC. The role of image guidance in improving the safety of pain treatment. Curr Pain Headache Rep. 2012 Feb;16(1):9-18.
Rimeika G, Saba L, Arthimulam G, Della Gatta L, Davidovic K, Bonetti M, Franco D, Russo C, Muto M. Metanalysis on the effectiveness of low back pain treatment with oxygen-ozone mixture: Comparison between image-guided and non-image-guided injection techniques. Eur J Radiol Open. 2021 Dec 6;8:100389.
Sage W, Pickup L, Smith TO, Denton ER, Toms AP. The clinical and functional outcomes of ultrasound-guided vs landmark-guided injections for adults with shoulder pathology–a systematic review and meta-analysis. Rheumatology (Oxford). 2013 Apr;52(4):743-51.
Sakellariou G, Conaghan PG, Zhang W, Bijlsma JWJ, Boyesen P, D’Agostino MA, Doherty M, Fodor D, Kloppenburg M, Miese F, Naredo E, Porcheret M, Iagnocco A. EULAR recommendations for the use of imaging in the clinical management of peripheral joint osteoarthritis. Ann Rheum Dis. 2017 Sep;76(9):1484-1494.
Strakowski JA, Visco CJ. Diagnostic and therapeutic musculoskeletal ultrasound applications of the shoulder. Muscle Nerve. 2019 Jul;60(1):1-6.
Wang H, Zhu Y, Wei H, Dong C. Ultrasound-guided local corticosteroid injection for carpal tunnel syndrome: A meta-analysis of randomized controlled trials. Clin Rehabil. 2021 Nov;35(11):1506-1517.
Wu T, Song HX, Dong Y, Li JH. Ultrasound-guided versus blind subacromial-subdeltoid bursa injection in adults with shoulder pain: A systematic review and meta-analysis. Semin Arthritis Rheum. 2015 Dec;45(3):374-8.
Yang FA, Shih YC, Hong JP, Wu CW, Liao CD, Chen HC. Ultrasound-guided corticosteroid injection for patients with carpal tunnel syndrome: a systematic review and meta-analysis of randomized controlled trials. Sci Rep. 2021 May 17;11(1):10417.